What is Thalassemia?
Thalassemia is a blood disorder passed down through families (inherited) in which the body makes an abnormal form of hemoglobin, the protein in red blood cells that carries oxygen. The disorder results in excessive destruction of red blood cells, which leads to anemia. Anemia is a disorder in which your body doesn’t have enough normal, healthy red blood cells (RBC).
This disease is inherited, meaning that at least one of your parents must be a carrier of the disease. It is caused by either a genetic mutation, or a deletion of certain key genes.
Causes and Risk Factors for Thalassemia
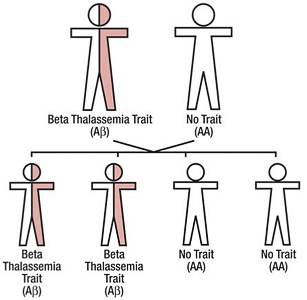
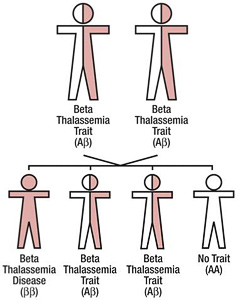
Thalassemia occurs when there is an abnormality or mutation in one of the genes involved in hemoglobin production. This genetic defect is inherited from your parents. If only one of your parents is a carrier for thalassemia, you may develop a form of the disease called “thalassemia minor.” If this occurs, you will probably not have symptoms, but you will be a carrier of the disease. Some people with thalassemia minor do develop minor symptoms. If both of your parents are carriers of thalassemia, you have a 25 percent chance of inheriting a more serious form of the disease.
Thalassemia is most common in people from Southeast and Central Asia, the Mediterranean, the Middle East, India, and North Africa. Thalassemia is most common in people from Southeast and Central Asia, the Mediterranean, the Middle East, India, and North Africa.
How Are Thalassemia Diagnosed?
Doctors diagnose thalassemia using blood tests, including a complete blood count (CBC) and special hemoglobin tests. A CBC measures the amount of hemoglobin and the different kinds of blood cells, such as red blood cells, in a sample of blood. People who have thalassemia have fewer healthy red blood cells and less hemoglobin than normal in their blood. People who have alpha or beta thalassemia trait may have red blood cells that are smaller than normal.
Hemoglobin tests measure the types of hemoglobin in a blood sample. People who have thalassemia have problems with the “alpha” or “beta” globin protein chains of hemoglobin. Moderate and severe thalassemia usually diagnosed in early childhood. This is because signs and symptoms, including severe anemia, often occur within the first 2 years of life. People who have milder forms of thalassemia might be diagnosed after a routine blood test shows they have anemia. Doctors might suspect thalassemia if a person has anemia and is a member of an ethnic group that is at increased risk for thalassemia. Doctors also test the amount of iron in the blood to find out whether the anemia is due to iron deficiency or thalassemia. Iron-deficiency anemia occurs if the body does not have enough iron to make hemoglobin. The anemia in thalassemia occurs because of a problem with either the alpha globin or beta globin chains of hemoglobin, not because of a lack of iron. Because thalassemia are passed from parents to children through genes, family genetic studies also can help diagnose the disorder. These studies involve taking a family medical history and doing blood tests on family members. The tests will show whether any family members have missing or altered hemoglobin genes.
What Are the Symptoms of Thalassemia?
The symptoms of thalassemia depend on which type you have:
Thalassemia minor:
Thalassemia minor usually does not cause any symptoms. If it does, it causes only minor anemia.
Beta thalassemia:
Beta thalassemia comes in two serious types:
- Thalassemia major.
- Thalassemia intermedia.
The symptoms of thalassemia major generally appear before a child’s second birthday. The severe anemia related to this condition can be life-threatening.
Other symptoms include:
- Breathing difficulties
- Paleness
- Frequent infections
- Poor appetite
- Jaundice (yellowing of the skin and whites of the eyes)
- Enlarged organs
- Dark urine
This form of thalassemia is usually so severe that it requires regular blood transfusions.
Thalassemia intermedia is a less severe form of beta thalassemia. While people with this condition still have anemia, they do not need blood transfusions.
Alpha Thalassemia:

Alpha thalassemia also has two serious types:
- Hemoglobin H disease
Hemoglobin H disease can cause bone issues. The cheeks, forehead, and jaw may all overgrow. In addition to the bone issues and the anemia associated with any kind of thalassemia, hemoglobin H disease can cause these other symptoms:
- jaundice
- extremely enlarged spleen
- malnourishment
- Hydrops Fetalis
Hydrops Fetalis is an extremely severe form of thalassemia. It occurs before birth, and most individuals with this condition are either stillborn or die shortly after being born.
How is Thalassemia Treated?
The treatment for thalassemia depends on the type and severity of disease involved. Your doctor will give you a course of treatment that is customized to your particular case In general,
treatments you may receive include
Treatment may include:
- Blood transfusions
- Bone marrow transplant
- Medications and supplements
- Possible surgery to remove the spleen and/or gallbladder
Prevention:
In most cases, thalassemia can't be prevented. If you have thalassemia, or if you carry a thalassemia gene, consider talking with a genetic counselor for guidance before you have a child.
Premarital Tests are very important to prevent thalassemia, especially for those who carry the gene but do not experience any thalassemia symptoms.
Resources:
http://www.healthline.com/
http://www.moh.gov.sa/
http://www.nhlbi.nih.gov/